What is Neuro-Linguistic Programming?
Neuro-linguistic programming is a psychological approach which asserts that one can adapt strategies used by successful individuals to achieve one’s own goals. It guides the individual in learning from their own experiences of success and failure about which thoughts, feelings, and behaviors are useful, and which are getting in their way. No action is negative, even if it leads to perceived failure, as it is just a step in the learning process.
History and Origins of Neuro-linguistic Programming (NLP)
Although Jon Grinder and Richard Bandler often receive most of the credit for originating Neuro-Linguistic Programming, NLP was actually founded by a group of people who made consistent contributions. This group includes Grinder and Bandler as well as Frank Pucelik, Robert Dilts, Judith Delozier, Leslie Cameron, David Gordon, and others.
At the University of California, Santa Cruz in early 1970s this enlightened group set out to discover the specific communication patterns that enabled outstanding psychotherapists such as Milton Erickson (famous psychiatrist/hypnotherapist), Virginia Satir (founder of Family Systems Therapy), and Fritz Perls (founder of Gestalt Therapy) to achieve uncommon results with their clients. By direct observation and videotape analyses, they were able to break down these practitioners’ effective patterns of communication and teach them to others.
The process used to discover the magic in transformative communication was called modelling. Many consider modelling to be the heart and soul of Neuro-Linguistic Programming. When you know how to create models based on the expertise of others, you can learn and teach any new skill in its essential form.
NLP has its roots in the field of behavioural science, developed by Pavlov, Skinner and Thorndike. It uses physiology and the unconscious mind to change thought processes and therefore behaviour.
NLP fundamentally state that everyone’s born with the same basic neurology. Our ability to do anything in life, whether it’s swimming the length of a pool, cooking a meal, or reading a book depends on how we control our nervous system. So, much of NLP is devoted to learning how to think more effectively and communicate more effectively with yourself and others.
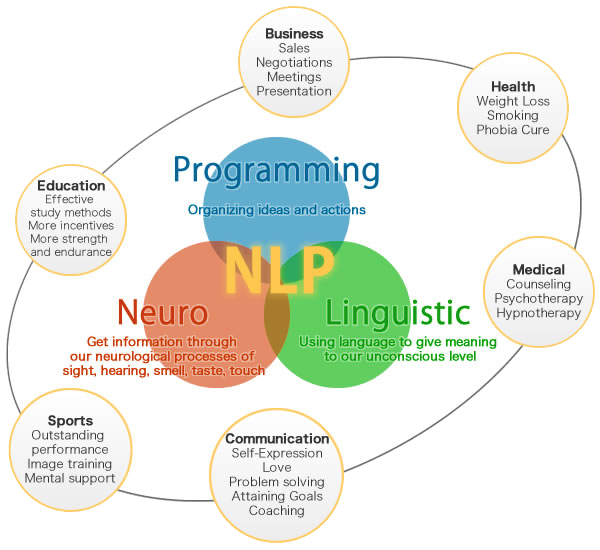
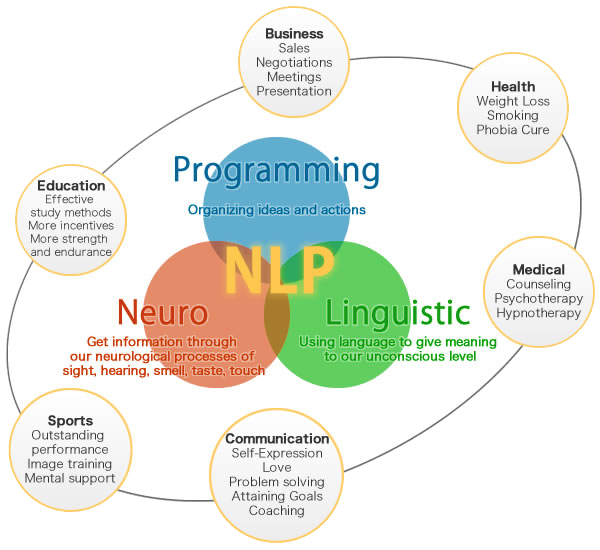
Neuro is about your neurological system. NLP is based on the idea that we experience the world through our senses and translate sensory information into thought processes, both conscious and unconscious. Thought processes activate the neurological system, which affects physiology, emotions and behaviour. NLP teaches a structural way of viewing mind and body states, developing mental maps that show how things happen and how to change course.
Linguistic refers to the way human beings use language to make sense of the world, capture and conceptualise experience, and communicate that experience to others. In NLP, linguistics is the study of how the words you speak influence your experience. Language is the tool we use to gain access to the inner workings of the mind. Neuro-linguistic programming language patterns teach us how to access unconscious information that would remain vague and unknowable otherwise.
Programming refers to the capacity to change our mind and body states. Programming draws heavily from learning theory and addresses how we code or mentally represent experience. Your personal programming consists of your internal processes and strategies (thinking patterns) that you use to make decisions, solve problems, learn, evaluate, and get results. NLP shows people how to recode their experiences and organize their internal programming so they can get the outcomes they want. You’ve heard the term living on autopilot, right? To someone trained in NLP, this would mean that you are living according to your programming, which consists of habitual thoughts, feelings, reactions, beliefs, and traditions. Someone trained in Neuro-linguistic programming knows how such programs are structured in the mind and how to access them through conversation (language) so that outdated programs and autopilot behaviors can be changed.
By assessing a person’s speech, actions, thoughts, and feelings, Neuro-linguistic programming practitioners build an understanding of the person’s map of reality. NLP techniques are then used to help the person copy the processes used by others, to use them in place of techniques that have not proved successful.
Since it was conceived in the 1970s, Neuro-linguistic programming (NLP) has interested professionals and laymen alike, with its simple and practical therapy methods. The practice makes use of the way an individual’s mind works to change responses to thoughts and feelings. Some of its techniques have become entangled with popular culture, such as the so-called ability to detect lies by watching a person’s eye movements.
Neuro Linguistic Programming (NLP) is all about bringing about changes in perception, responsible communication and developing choices of responses or communication in a given situation. The situation can be personal or professional, but it empowers you by giving you choices and also being responsible for the choice made by you.
NLP believes in perfection of nature in human creation. Hence NLP encourages the client to recognize their sensory sensitivities and use them to respond to a particular problem. In fact, NLP also believes that the mind is capable of finding even cures to ailments and diseases.
How does Neuro-Linguistic Programming suggest the mind works and how does NLP work in real life?
During conversations, most of us fixate on words. What does this person mean and what shall I say in return? It’s been long established that words are the least meaningful aspect of communication, conveying just 7% of meaning (Mehrabian, 1972).
For example, when someone tells you they’re willing to help you organize a social gathering, but their voice is flat and their facial expression looks like you just invited them to an evening of electric shock torture…it’s obvious something else is going on. Their words said YES, but the non-verbal communication – the other 93% – said SOMETHING ELSE.
What is Neuro-Linguistic Programming? The other 93% of communication. NLP is a system for understanding and using the communication that really matters. Master non-verbal communication and you become a communication master!
But here’s something even more interesting:
Most people don’t realize that communication is made of so much more than interactions between people. There exists an entire world of communication within your mind and body. Inner life – your mindset, attitude, and feelings – is an active form of communication.
NLP suggests that each individual’s mind creates a map of the world, using data received through the senses. Each individual’s maps are different, with varying levels of importance placed on input from different senses. For example, some people understand the world based more on their visual perceptions, while others understand it based more on their auditory perceptions.
The system that the person uses to process experiences is called a primary representational system (PRS), and knowledge of it is essential to accessing and changing the individual’s personal map.
Neuro-linguistic programming techniques work on the assumption that the PRS can be enlisted to influence the individual’s map.
NLP might appear like magic or hypnosis. During therapy the subject goes deep into their unconscious mind and sifts through layers and layers of beliefs and perceptions to become aware of an experience in early childhood that is responsible for a behaviour pattern. NLP works on the principle that everyone has all the resources they need to make positive changes in their own life. NLP techniques are used as a tool to facilitate these changes.
NLP Therapy can be content free. That means the therapist can be effective without knowing about the problem in great detail. Hence the therapist need not be told about the event or even the issue, thereby ensuring privacy for the client. Besides this we also have a non- disclosure agreement in which the interaction between the client and the therapist is kept confidential.
NLP techniques involve non-invasive, medicine free therapy that helps the client discover new ways of dealing with emotional problems such as low self-esteem, anxiety, lack of confidence, destructive relationship patterns (coping with breakup), and are successful ineffective bereavement counselling.
The most important communication is not between people but within people.
Inner communication is a strong suit of Neuro-Linguistic Programming, which was originally known as the study of the structure of subjective experience. This is a fancy way of saying that NLP breaks down what’s going on between your ears so that you can do something constructive with it. Here’s a taste of how it works.
Let’s say you’re having friends over for dinner and you’re feeling extra tense. You’re not sure why. Everything seems fine, but you’re feeling on edge. An NLP Practitioner could figure out how you’re creating this tense state in a few moments. It’s all about how you’re communicating with yourself on the inside.
The NLP Breakdown of Inner Communication
Inner communication is made of images, sounds, and feelings (the NLP VAK Model). Finding out what’s giving you tense feelings is a matter of discovering which images and sounds go with the tense feeling. As you turn your attention inward, looking for what you see and hear on the inside, you might discover that you are imagining things about the dinner:
• You’re seeing your house all messy as the guests arrive. • An inner voice that says, “They’re going to hate your dinner.” • Looks of disgust on their faces as they eat. • You’re sitting alone in your house because no one showed up. And so on.
The point is: You probably weren’t consciously aware of all the inner communication channels. If you’re feeling tense about dinner, you’re probably imagining how badly it could go and responding to this unconscious imagery and sound. The tense feelings are a mirror of the other channels.
This is why Neuro-Linguistic Programming claims that people are not broken. We simply respond to inner communication, whether or not we’re aware of it. So, if you’re picturing bad things, happening at your dinner party, you’re going to feel tense. You’re working perfectly.
When you become aware of how you are perfectly creating a mindset you don’t want, you can change it. Neuro-Linguistic Programming offers a vast library of methods to change our mindset once we identify it. Transforming the inner communication so that you feel better is the Programming aspect of NLP.
How Does Neuro-Linguistic Programming Cause Change?
Neuro-linguistic programming causes change by improving one’s understanding of their cognitive and behavioural patterns. It also builds more effective communications between conscious and unconscious mental processes.
Once a person has a better understanding of their personal map of reality, they can analyze what is effective in achieving their goals and what is not. They can then analyze the perspectives of others and assess what leads to their success. NLP is primarily experiential, and therefore the individual has to perform an action in order to actually learn from the experience.
NLP practitioners focus on six logical hierarchies of learning, communication, and change. Each logical level organizes the data below it. Changes made at a lower level influence the higher levels, and vice versa.
The six logical levels in descending order are:
- Purpose and spirituality
- Identity
- Beliefs and values
- Capabilities and skills
- Behaviors
- Environment
What Happens in a Neuro-Linguistic Programming Session?
In an NLP therapy session, the therapist works with a person to understand his/her thinking, behaviors, emotional states, and aspirations. They then attempt to outline the person’s map of the world, along with their primary representational system (PRS). Once they have a foundation, they use a variety of techniques to change the way the person thinks, feels, or behaves in certain situations.
Neuro-linguistic programming has a firm foundation in Friz and Laura Perls’ Gestalt Therapy asks the individual to focus on the “here and now,” using their current thoughts and feelings, along with their relationship with the therapist, to identify what they’d like to change and to find solutions. Thus, NLP sessions are strongly based in the present, and require the client to work towards change in the session itself.
The NLP communication model
The NLP communication model is based on cognitive psychology and was developed by Richard Bandler and John Grinder. According to the NLP communication model, when someone behaves in a certain way (their external behaviour), a chain reaction is set up within you (your internal response), which in turn causes you to respond in some way (your external behaviour), which then creates a chain reaction within the other person (their internal response), and the cycle continues.

The internal response is made up of an internal process and an internal state. The internal process consists of self-talk, pictures, and sounds and the internal state is the feelings that are experienced.
 Pillars of NLP
Pillars of NLP
These are the four pillars (foundations) of the Neuro-linguistic programming
Rapport
NLP provides an important gift to build relationships with other people. Rapport can be described as connecting quickly with others. Creating rapport creates trust from others. Rapport can be built quickly through understanding modality preferences, eye accessing cues and predicates.
Sensory awareness
Sometimes when you walk into someone’s home, you notice that the colours, smells, and sounds are subtly quite different from yours. Neuro-linguistic programming enables you to notice that your world is much richer when you deliberately pay attention to your senses wholly.
Outcome thinking
An outcome is your goal for doing something. Outcome connects to thinking about what you want, as opposed to getting stuck in a negative mode of thinking. The principles of outcome approach may help to make the best decisions and choices.
Behavioural flexibility
Behavioural flexibility means being able to do something differently if the way you’re currently doing it isn’t working. Being flexible is a key aspect of practicing NLP. Learning NLP helps you to find fresh perspectives and to build these habits into your repertoire.
Techniques Used in Neuro-Linguistic Programming
NLP sessions use a variety of eclectic techniques, chosen according to the particular client’s PRS.
Some of the most common techniques include the following:
- Anchoring: associating an action as a trigger for certain emotional states. For example, the practitioner might help an individual immerse him/herself in a feeling of confidence, then ask them to do a repetitive action, such as squeezing the forefinger and thumb together. The idea is that this action will later trigger the sense of confidence.
- Rapport: the practitioner mirrors some of the client’s unconscious physical actions, creating a quick rapport and using empathy to better guide the client towards their goals. This is generally used in conjunction with other techniques, making them more powerful and effective.
- Swish pattern: the client is guided to visualize their regular patterns of behaviour or thought, and adjusts these patterns to lead to a desired outcome. For example the client visualizes a feeling such as anxiety, giving it a shape, size, and colour. They then monitor it as it spirals in its familiar direction. Once they have a vivid representation of it, they attempt to spiral it in the opposite direction, towards achieving a more useful result and feeling.
- Visual/kinaesthetic dissociation (VKD): this technique uses visualization and other strategies to dissociate negative thoughts and feelings with an event. This is often used for treating PTSD. The client visualizes the traumatic event as if it is a movie, viewing it from a safe distance. The client is then led to vividly visualize it ending in a safe place, rather than in the trauma.
- Association: some practitioners use the opposite of the previous technique. For example some therapist would treat bulimia by associating the vomiting process with repulsion. Since bulimic clients generally have no problem with vomiting, she guides them towards having a strong negative reaction towards it.
- Failure into feedback: this is a fundamental technique used in conjunction with other strategies. The client learns to see lack of success as feedback rather than failure.
What conditions can be treated using Neuro-Linguistic Programming?
| Proponents of Neuro-linguistic programming recommend its use for a number of mental health issues. These include anxieties and phobias, communication issues, Post Traumatic Stress Disorder, depression, attention disorders, addictions, schizophrenia, OCD, and borderline personality disorder. |
 |
Treatment of anxiety and phobias accounts for the most widespread use of NLP, seeing as it is particularly suited to eliminating negative associations with situations and behaviors.










 Pillars of NLP
Pillars of NLP
